No greater nightmare has probably crossed the minds of many women than discovering a lump in her breast. That little surprise change in your breast tissue can make you immediately anxious and nervous, with an onslaught of “what if” questions that practically cross your mind. Not every lump is malignant; indeed, many are not. Nevertheless, knowing what you have is crucial to both your peace of mind and your overall health.
The truth is that breast cancer has affected 1 in 8 women during her lifetime, making it one of the most common cancers throughout the globe. But here’s what is really reassuring: breast cancer diagnosed at its early stages has a stunning 98% survival rate.
Understanding breast lumps is just one part of a big picture of the state of breast health. If you want to know more about the causes of cancer, its symptoms, and how to treat it properly, here’s all in this comprehensive guide entitled “What is Cancer? Causes, Symptoms and Treatment.” Having a greater perspective can benefit you in making better decisions and understanding what steps to take concerning your health.
Whether you are newly diagnosed or you feel you need to know something about the health of your breasts now, this comprehensive guide will walk you through all the basics you need to know-from understanding different types of breast lumps to treatment options and life with a diagnosis. Now, let’s delve into the basics of breast lumps and breast cancers, beginning with just what is meant by the term breast lump, why some become serious concerns and others simply are not.
Understanding Breast Lumps
Typical Varieties of Breast Lumps
Breast lumps may be of two kinds-benign and malignant types. The classification can be given as follows:
| Type | Characteristics | Common Age Group | Risk Level |
| Fibroadenomas | Smooth, round, movable | 20-30 years | Benign |
| Cysts | Fluid-filled, soft | 30-50 years | Benign |
| Fibrocystic Changes | Multiple, tender | 30-50 years | Benign |
| Ductal Carcinoma | Hard, irregular, fixed | 40+ years | Malignant |
| Lobular Carcinoma | Thickening, subtle changes | 45+ years | Malignant |
Normal and Abnormal Breast Changes
Normal breast changes may include:
- Monthly cyclical changes brought about by hormones.
- Pregnancy-related changes
- Postmenopausal change
- General tenderness or lumpiness
Abnormal changes that warrant immediate attention:
- Hard, fixed masses
- Skin dimpling or puckering
- Nipple discharge (especially bloody)
- Sudden asymmetry
- Recurring pain in one place
If you’re concerned about whether these changes may be linked to breast cancer, it’s important to understand the broader picture. Learn more in our detailed guide on What is Breast Cancer? Causes, Symptoms, and Treatment.
Risk Factors for Forming Breast Lumps
Several factors can increase the risk of encountering breast lumps:
Key Risk Factors:
- Age (risk increases with age)
- Family history of breast cancer
- Personal history of breast diseases
- Dense breast tissue
- Genetic mutations, specifically (BRCA1 and BRCA2)
Lifestyle risk factors:
- Obesity
- Alcohol drinking
- Lack of physical activity
- Hormone replacement therapy
- Advanced pregnancy or absence of pregnancy
Age-Related Breast Changes
The breast tissue continues to change throughout life:
20s-30s:
- Thick, resilient breast tissue
- Fibroadenomas are very common
- Regular monthly changes
40s-50s:
- Increased fatty tissue
- Greater risk of cysts
- Perimenopause-related changes
Post-50s:
- Softer, less dense tissue
- Greater risk of malignancy tumors
- Decreased hormone-related changes
With age, systematic self-examinations of the breasts become more important. Changes in the composition of the tissue of the breast may also alter how lumps are detected and interpreted through screening. For those navigating life after breast cancer, challenges such as intimacy and sexual health may arise. Discover practical insights in our guide on Sexual Life after Breast Cancer. Finally, we will review certain signs and symptoms that may indicate a concerning breast condition.
Signs and Symptoms
Characteristics of Cancerous Lumps
A cancerous breast lump usually has several characteristic features distinguishing it from a benign mass:
- Texture and Feel
- Hard or firm consistency
- Irregular or asymmetrical shape
- Poor mobility (stuck to tissues)
- Generally painless
- Incompressible
| Feature | Cancerous Lump | Benign Lump |
| Shape | Irregular | Round/Oval |
| Edges | Poorly defined | Well-defined |
| Movement | Fixed | Mobile |
| Texture | Hard | Soft/rubbery |
| Growth | Progressive | Stable |
Pain and Tenderness
Although most breast cancers are initially painless, some women might experience:
- Intermittent or persistent discomfort
- Tenderness that doesn’t correlate with menstrual cycle
- Sharp, stabbing pain in the breast region
- Unusual feelings in the breast or underarm
Skin Changes and Dimpling
The visible alterations in the breast may be an important sign of masked cancer:
Surface Changes:
- Peau d’orange (skin like an orange peel)
- Dimpling or puckering
- Redness or swelling
- Scaling or flaking of the nipple area
- Visible venous patterns
Nipple Changes:
- Inversion or retraction
- Discharge (especially bloody)
- Changes in nipple direction
- Crusting or ulceration
These symptoms can appear alone or together, and their occurrence does not necessarily imply cancer. However, the simultaneous presence of some of these symptoms increases the likelihood of malignancy. Did you know that breast cancer doesn’t only affect women? Learn more about Male Breast Cancer and how it manifests. Additionally, some symptoms of breast cancer might be subtle or overlooked. Explore this Hidden Symptoms of Breast Cancer to stay informed about what to watch for. Some women may notice these changes during their daily self-exams, while others may discover them accidentally as part of their everyday routine.
Now that you know the most common signs and symptoms, let’s discuss how these findings serve as the basis for the diagnosis of breast cancer through diagnostic procedures
Diagnostic Process
Self-examination Techniques
The first tool for early detection of abnormalities in the breast is self-checking. Perform these checks monthly, using the three basic techniques herein:
- Visual inspection in front of mirror
- Manual examination while standing
- Manual examination while lying down
Clinical Breast Examination
Healthcare providers perform full physical examinations, employing:
- Systematic palpation techniques
- Lymph nodes assessment
- Size and location of abnormalities are documented
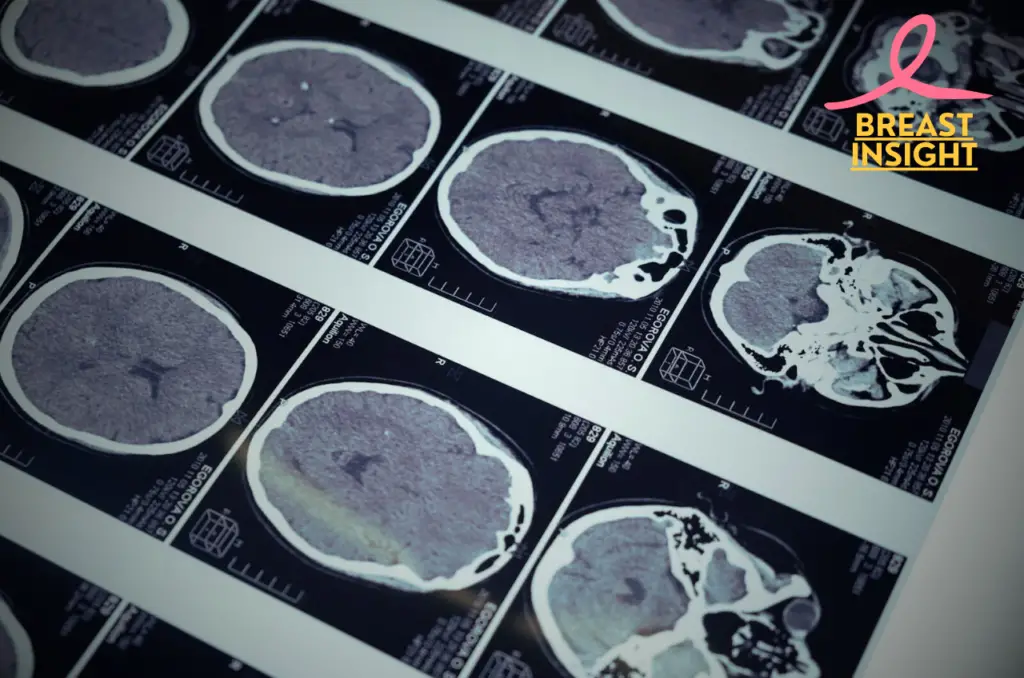
Imaging Tests
A number of imaging techniques are used to diagnose and evaluate breast lumps:
| Test Type | Purpose | Best Used For |
| Mammogram | X-ray imaging | Initial screening |
| Ultrasound | Sound wave imaging | Dense breast tissue |
| MRI | Detailed soft tissue imaging | High-risk cases |
| 3D Mammography | Advanced X-ray | Complex cases |
Biopsy Techniques
Other biopsy techniques are available, depending on where suspicious areas are felt:
- Fine-needle aspiration (FNA)
- Quick procedure
- Low invasion
- Uses thin needle
- Core needle biopsy (CNB)
- Removes tissue sample
- Local anesthesia
- Larger than FNA
- Surgical biopsy
- Removes entire lump
- Most resolved results
- Performed under general anesthesia
Understanding Exam Outcomes
Test results typically include:
- Tissue classification (benign vs. malignant)
- Hormone receptor status
- HER2 status
- Staging and grading if malignancy exists
Interpretation of results
- Pathology report analysis
- Staging classification if warranted
- Treatment planning discussions
- Risk assessment evaluation
The diagnostic process requires careful coordination between different medical specialists, including radiologists, pathologists, and oncologists. Each step builds upon previous findings to create a comprehensive understanding of the breast abnormality. This thorough approach ensures accurate diagnosis and appropriate treatment planning.
Understanding the stages of breast cancer is a crucial next step in tailoring effective treatments. To learn more, visit our guide on Stages of Breast Cancer Every Woman Should Know.
Having clear understanding diagnostic process, we will now turn our attention to the many treatment options available based on different types of breast lumps and cancer diagnoses.

Treatment Options
Surgical interventions
The mainstay for tumor removal remains, however, surgical treatment. Surgical intervention will largely depend on the characteristics of the tumor, such as tumor size, location, and stage of its development.
- Lumpectomy: Removal of tumor and surrounding tissue while preserving breast
- Mastectomy: Complete removal of breast tissue
- Sentinel node biopsy: Removal of first lymph nodes where cancer cells likely spread
- Axillary lymph node dissection: Typically includes removal of several lymph nodes
Radiation Therapy
Radiation therapy employs high-energy beams designed to precisely target and annihilate cancer cells, usually given following surgery to eradicate any lingering cancerous cells.
| Type | Duration | Application |
| External beam | 3-6 weeks | Applied from outside the body |
| Brachytherapy | 5-7 days | Internal radiation via catheters |
| Intraoperative | One-time | During surgery |
Chemotherapy options
Chemotherapy is prescribed either before surgery (neoadjuvant) or after it’s performed (adjuvant), according to the cancer stage and type.
Common chemotherapy protocols include:
- Anthracyclines (doxorubicin, epirubicin)
- Taxanes (paclitaxel, docetaxel)
- Cyclophosphamide
- 5-fluorouracil
Targeted therapies
Target therapy-cancer cell kills with reduced collateral to normal cells.
- HER2-targeted drugs: Trastuzumab, pertuzumab
- Hormone therapy options:
- Tamoxifen in pre/post-menopausal women
- Aromatase inhibitors for post-menopausal females
- CDK4/6 inhibitors: Palbociclib, ribociclib
- PARP inhibitors: For BRCA-mutated cancers
Treatment effectiveness varies among patients, and doctors typically combine multiple approaches for optimal results. The choice of treatment depends on:
- Cancer stage and grade
- Hormone receptor status
- HER2 status
- Patient’s age and general well-being
- Personal preferences
Side effects management is, therefore, essential in the treatment process; health care teams work closely with patients to minimize complications while maximizing treatment effectiveness.
To learn more about managing the lesser-known challenges of radiation therapy, visit our guide on Real Side Effects of Radiation Therapy.
Having discussed above the different options of treatment, let us focus on how to live daily life handling the breast cancer and its associated treatments.

Living with Breast Cancer
Coping Strategy
- Practice mindfulness and meditation to handle anxiety
- Join breast cancer support groups
- Keep a journal to process your emotions
- Seek professional counseling whenever needed
- Set realistic daily goals and celebrate small victories
Support Systems
Support systems are very important for patients with breast cancer. Here is a wide range of the support available:
| Support Type | Benefits | Examples |
| Family & Friends | Emotional comfort, daily assistance | Help with chores, accompaniment to appointments |
| Professional | Medical guidance, mental health support | Oncologists, therapists, social workers |
| Community | Shared experiences, practical advice | Support groups, online forums, advocacy organizations |
Follow-up Care
Consistent follow-up care is vital for sustaining long-term health:
- Schedule regular mammograms and imaging tests
- Maintain detailed records of symptoms and side effects.
- Attend all scheduled appointments with your healthcare team
- Monitor for signs of recurrence or new symptoms
- Routine physical examination every 3-6 months for the first three years
Lifestyle Changes
Healthy lifestyle changes can improve the quality of life and help in recovery.
Physical Activity:
- Begin with easier workouts such as walking or yoga
- Gradually build activity
- Continue strength training, if advised by health care provider
- Try to make 150 minutes of moderate activity in a week
Nutrition:
- Focus on plant-based foods
- Get enough protein
- Stay hydrate
- Reduce drinking
- Avoid processed foods
Stress Management:
- Establish regular sleep patterns
- Practice relaxation techniques
- Establish boundaries at work and at home
- Engaging in enjoyable hobbies
Social Connections:
- Maintain connections with loved ones
- Join survivor networks
- Participate in community functions
- Share experiences when comfortable
Recovery is very individual for each person. Working closely with your healthcare team allows for the establishment of a personalized plan that incorporates both your specific situation and your requirements. By following these strategies and keeping in communication with your doctors, you are best placed to attain the highest quality of life during and after your treatment.
To explore the best treatment options that complement these strategies, visit Best Breast Cancer Treatments. Having discussed the process of living with breast cancer, it is important to recognize that each situation is different and that all these models can be tailored to individual requirements and circumstances.

Conclusion
Finding a breast lump can become a turning point in life, but education combined with early intervention proves to be a powerful companion in the fight against breast cancer. With an understanding of the different kinds of breast lumps, it pays to note red flags, and it seeks an accurate diagnosis, it empowers you to take charge of your journey. Widespread treatment options and advanced diagnostic methods are bringing hope and improving outcomes for the many touched by this disease.
While it is important to note that most breast lumps are not malignant, all changes in your breast tissue must be evaluated by a healthcare provider. Self-assessment, regular mammograms, and a discussion with your health care provider are some very important steps for maintaining the health of your breasts. You’re never alone when you have a breast condition or want to be proactive; a strong network of medical professionals, support groups, and resources are ready to help you navigate along the way.
Frequently Asked Questions (FAQs)
What are the most common types of breast lumps?
There are two major categories of breast lumps: benign and malignant. Some of the most common benign lumps include fibroadenomas, cysts, and lipomas. Malignant lumps are most often associated with breast cancer. For this reason, any new lump found should be evaluated by a healthcare provider to determine what its nature is and how it should be managed.
How can I perform breast self-examination?
To administer the BSE, follow these steps:
1. Look in the mirror and make sure that your breasts have not become lumpy or inflamed differently in shape or size.
2. Lift the arms high, and examine the skin of the breasts for any abnormality.
3. Lie down and press the pads of your fingers against the breast, feeling out lumps or any other abnormalities in a circular motion over the whole breast.
4. This process continues, whether standing or sitting, ensuring that every little bit of breast tissue is surveyed.
When should I see a doctor about a breast lump?
You should see a doctor if you notice any changes in your breasts, such as the presence of a new lump, persistent pain, or any change in the skin, including redness or dimpling. Rapidly growing lumps, or unusual nipple discharge, also require immediate medical attention, so early evaluation helps with effective diagnosis and treatment.
Are all breast lumps cancerous?
No, all breast lumps are not cancerous; in fact, most are benign, meaning they are non-cancerous. However, only a healthcare professional can provide an exact assessment and diagnosis. Imaging tests along with biopsies may be required to determine the nature of the lump in question and establish if any further action should be taken.

